4 min read
How to Eliminate Cord Chaos & Contamination in the OR, Part 1: Safety Risks of Poor Cord Management
Domico Med-Device Updated on December 2, 2024
This is Part 1 in a 3-part series on strategic cord management in the operating room. In Part 1, we’ll offer an overview of the safety risks of poor cord management.
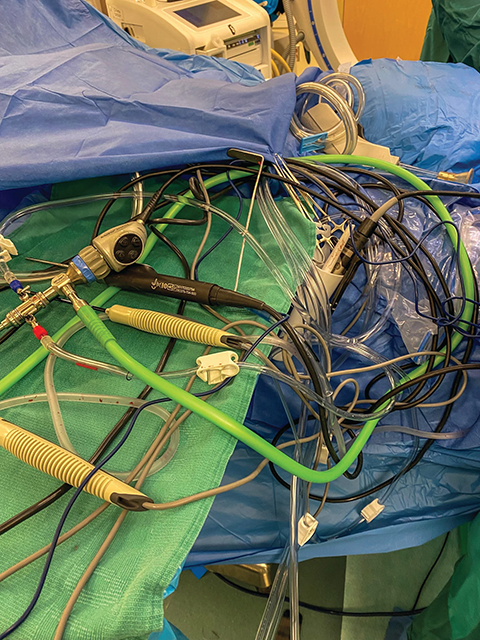
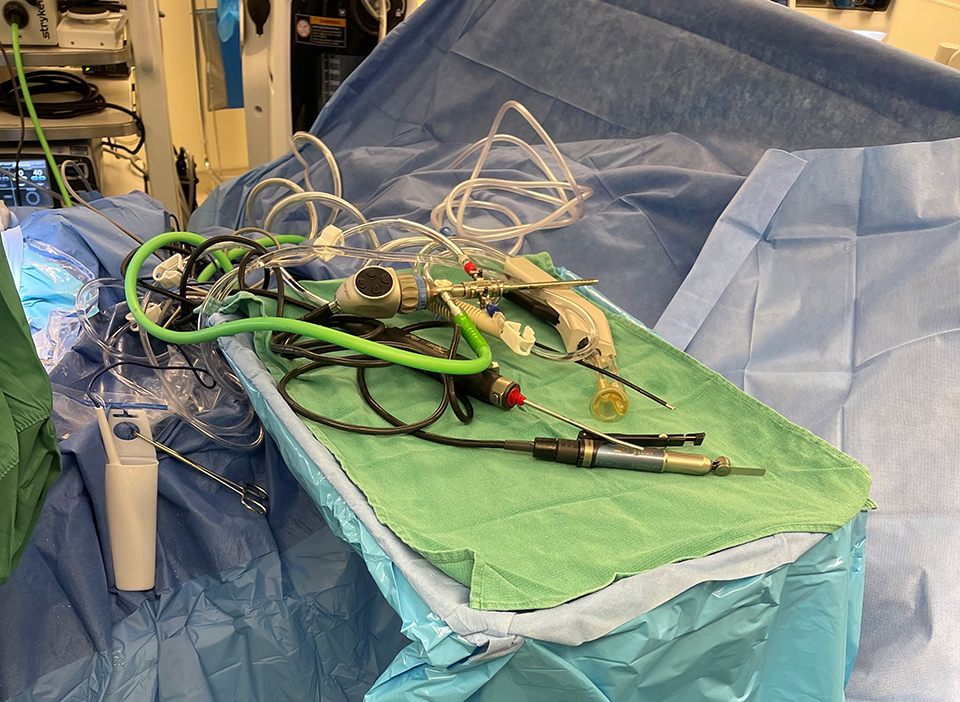
Surgical teams rely on many tools to deliver lifesaving and life-improving care, and most of those tools have cords. Arthroscopic, orthopedic, sports medicine, and ENT procedures often require multiple cords and even added cords throughout the surgery.
As critical as these tools are, they can prove difficult to manage, as cords are often a tangled mess that hinders efficiency, waste money, and even jeopardize safety. This series details how to eliminate cord chaos and contamination in the operating room for safer, more efficient, and cost-effective surgeries, starting with an overview of the safety risks of poor cord management.
Safety Risks of Poor Cord Management
Poor cord management in the surgical suite creates three unnecessary safety risks: contamination, prolonged anesthesia, and fire hazards.
1. Contamination
Additionally, tangled cords not only pose a risk of contamination during surgery but can also lead to delays in the procedure. Surgeons pulling on cords to adjust their position or length can inadvertently cause them to slip out of the sterile field, potentially introducing harmful bacteria or pathogens. This risk is further compounded when long apparatuses like bovies, burners, or shavers are involved, as they can easily fall out of the sterile area and contaminate the surgical site if not carefully managed.
Moreover, the use of metal clamps on PT drapes to secure cords can create a hazard in itself. These clamps, while effective in managing cords, can be sharp and tear the drapes if pulled forcefully, compromising the sterile environment. To address this issue, leading organizations like the Association of periOperative Registered Nurses (AORN) and the Association of Surgical Technologists (AST) recommend the use of non-metal clamps for cord management to prevent such incidents.
Furthermore, the risk of contamination extends beyond the surgical site to caregivers involved in post-operative cleanup. Tangled cords can inadvertently flick fluids onto healthcare workers during the cleaning process, increasing the likelihood of exposure to potentially infectious materials. This not only poses a health risk to the caregivers but also highlights the importance of proper cord management in maintaining a safe and sterile surgical environment.
These real-world risks underscore the critical importance of effective cord management practices in the operating room. By addressing these challenges proactively and implementing strategic solutions, healthcare facilities can minimize the risk of contamination, reduce surgical delays, and enhance the overall safety and efficiency of surgical procedures.
2. Prolonged Anesthesia
Furthermore, the replacement of contaminated tools and cords during surgeries not only causes delays but also adds to the complexity of the procedure. Falling instruments delay surgeries by an average of 7.6 minutes. In some situations where the entire field must be replaced due to contamination, surgical teams must navigate the challenge of re-establishing a sterile environment, further extending the time patients are under anesthesia.
The correlation between anesthesia duration and post-operative complications is a critical consideration in surgical settings. For example, a study of 2,196 patients concluded that longer anesthesia is associated with an increase in perioperative complications and mortality (National Center for Biotechnology Information), while another study of more than 3,800 patients found that prolonged anesthesia duration is associated with increased odds of complications, longer hospital stays, and a greater chance of returning to the OR (NCBI). Multiple studies suggest a link between anesthesia duration and the risk of complications. Yet another study suggests a link between prolonged anesthesia and neurotoxicity in the elderly and recommends limiting the duration of anesthesia whenever possible (NCBI).
Addressing the implications of prolonged anesthesia through effective cord management is essential for optimizing patient outcomes and reducing the risk of postoperative complications. By implementing strategic cord management practices, healthcare facilities can enhance the safety, efficiency, and overall success of surgical procedures, ultimately prioritizing the well-being of both patients and healthcare providers.
3. Fire Hazards
Operating room fires are a serious and potentially life-threatening risk that can occur during surgical procedures. The American Association of Nurse Anesthesiology reports that there are between 550 to 600 operating room fires each year, with the majority being preventable.
According to the American Society of Anesthesiologists, surgical fires require three key elements to ignite: an ignition source, such as electrosurgical units, lasers, and fiber optic light sources (many of which are corded), a fuel source like surgical drapes, alcohol-based skin prep, and patient hair, and an oxidizer such as oxygen, nitrous oxide, or even room air.
It is important to note that surgical energy, particularly monopolar radiofrequency energy (commonly referred to as the bovie), is the primary ignition source in 90% of operating room fire claims. Additionally, certain cords, such as those connected to light sources that generate heat, can also serve as potential ignition sources.
Proper cord management in the operating room is crucial for mitigating the risk of fires. By keeping cords organized, secure, and away from potential fuel sources, oxidizers, and ignition sources, the likelihood of accidental ignition is significantly reduced. This proactive approach to cord management not only promotes a safer surgical environment for both patients and healthcare providers but also helps prevent unnecessary and dangerous operating room fires.
Proper Cord Management Mitigates Safety Risks
Proper cord management can significantly reduce the risk of contamination, prolonged anesthesia, and fires by implementing strategic and smart practices.
-
Contamination: By organizing cords systematically and ensuring they remain within the sterile field, the risk of contamination is minimized. Surgeons and caregivers can navigate the surgical environment more efficiently without compromising sterility, ultimately reducing the likelihood of introducing harmful pathogens.
-
Anesthesia: Efficient cord management streamlines the surgical process, eliminating delays that may arise from tangled or misplaced cords. This not only reduces the time patients spend under anesthesia but also enhances the overall safety and success of the procedure by maintaining a consistent and controlled environment.
-
Fires: Effective cord management plays a crucial role in preventing operating room fires by minimizing cross-contact between potential fuel sources, oxidizers, and ignition sources. By keeping cords organized and secure, the risk of accidental ignition is significantly reduced, ensuring a safer surgical environment for both patients and healthcare providers.
Next Step
Discover how cord management increases operating room efficiency in Part 2 of this series.

An Overview of Surgical Table Accessories
Patient safety is the cornerstone of any successful surgical procedure, and ensuring the well-being and stability of patients is a top priority for...
How to Eliminate Cord Chaos & Contamination in the OR, Part 2: How Cord Management Increases Efficiency
This is Part 2 in a 3-part series on strategic cord management in the operating room. Part 1 offered an overview of the safety risks of poor cord...