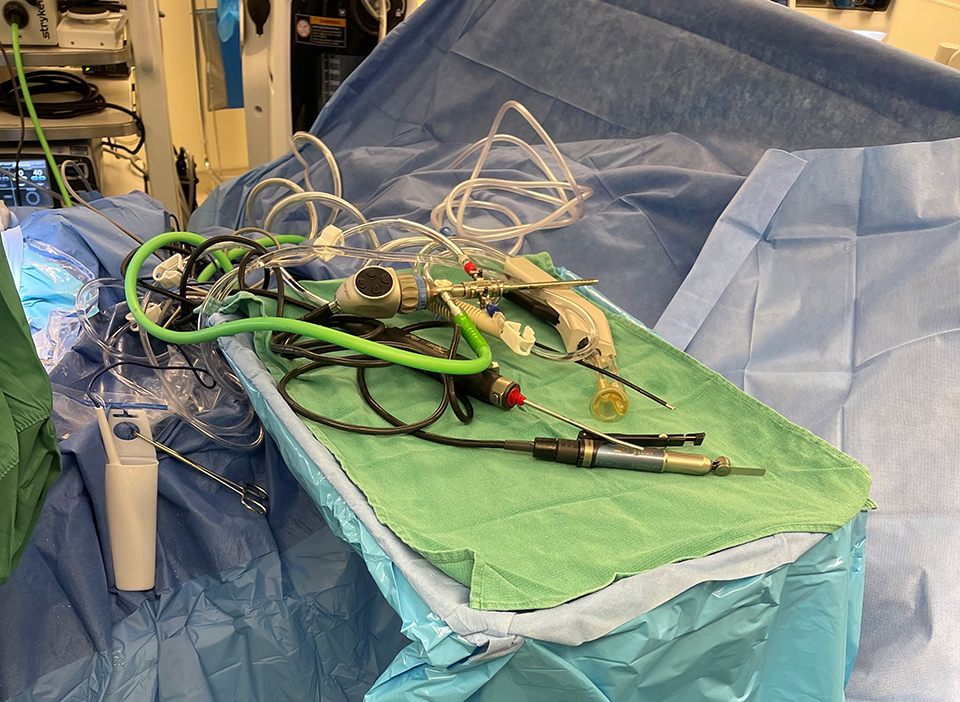
How to Eliminate Cord Chaos & Contamination in the OR, Part 1: Safety Risks of Poor Cord Management
This is Part 1 in a 3-part series on strategic cord management in the operating room. In Part 1, we’ll offer an overview of the safety risks of...
4 min read
Domico Med-Device Updated on December 2, 2024
This is the final installment in a 3-part series on strategic cord management in the operating room. Part 1 offered an overview of the safety risks of poor cord management. Part 2 discussed how cord management increases efficiency. In Part 3, we’ll explain how cord management reduces costs.
Strategic cord management not only improves patient and caregiver safety while increasing operating room efficiency, but it can also save patients and hospitals money. Here’s how.
Strategic cord management saves money by reducing surgical time, eliminating broken tools and cords, speeding set up and turnover time, and decreasing infection risk.
Surgeries get delayed when metal clamps tear PT drapes or tools and cords leave the sterile field and need to be replaced. Falling instruments add an average of 7.6 minutes to each surgery. Considering the average orthopedic procedure costs $60 to $100 per minute, that amounts to an additional cost of $456 to $760 per surgery.
Every minute in the operating room is valuable, and even minor delays can lead to significant cost implications. Surgical delays also increase anesthesia time, which is typically billed at one unit cost every 15 minutes. Replacing an entire sterile field, including cords and tools, can cost hospitals and patients thousands of dollars. Additionally, these delays can cascade, affecting subsequent surgeries and leading to a backlog of procedures.
Replacing contaminated cords and tools is expensive. For example, a single burner can cost $130. Strategic cord management keeps cords organized, reducing opportunities for damage and prevents tools from falling out of the sterile field, eliminating the need to replace them during surgery. Furthermore, the cost of frequently replacing damaged or contaminated instruments can quickly add up, straining hospital budgets and increasing the overall cost of healthcare delivery.
Beyond the financial costs, frequent replacement of tools and cords can disrupt the flow of surgery, causing distractions and potentially compromising the quality of care provided. Maintaining an organized and efficient surgical environment through strategic cord management minimizes these risks, ensuring that surgeries proceed smoothly and safely.
Proper cord management prevents tangles and enables techs to quickly set up, tear down, and clean up between procedures. This reduces downtime and allows hospitals to serve more patients and schedule more surgeries – eliminating waste and increasing revenue. A streamlined setup process not only saves time but also reduces the stress and workload on operating room staff, contributing to a more efficient and effective surgical team.
The ability to quickly and efficiently transition between surgeries is particularly important in high-volume surgical centers where multiple procedures are performed daily. By minimizing the time required for setup and turnover, hospitals can maximize their surgical capacity, ultimately leading to better utilization of resources and improved patient care.
Surgical Site Infections (SSIs) account for 20% of all healthcare-associated infections, costing hospitals an estimated $3.3 billion annually. SSIs also extend hospital stays by an average of 9.7 days, increasing the cost of hospitalization by more than $20,000 due to infections.
Infections not only have a significant financial impact but also pose serious health risks to patients. By decreasing the risk of SSIs, strategic cord management can reduce hospital stays, help hospitals avoid potential liabilities and lawsuits, and save both hospitals and patients money. Implementing effective cord management practices is a crucial step in enhancing infection control measures and ensuring a safe and sterile surgical environment.
Moreover, reducing the incidence of SSIs can improve patient outcomes and satisfaction, leading to better overall healthcare experiences. Hospitals that prioritize infection prevention through proper cord management are more likely to build trust with patients and enhance their reputation for providing high-quality care.
Consider your cord management practices. Are they standardized? Do caregivers use towels, metal clamps, or other “solutions” to manage cords? Are cords a chaotic mess during surgery? Is poor cord management a potential liability for patients, caregivers, and your organization?
Once you’ve evaluated your current practices, identify opportunities to improve patient and caregiver safety, conduct more efficient surgeries, and reduce OR costs via strategic cord management. Implementing standardized cord management protocols can help create a safer and more organized operating room environment.
Investing in specialized cord management systems designed for surgical environments can make a significant difference. These systems are specifically engineered to keep cords organized, secure, and out of the way, minimizing the risk of contamination and damage. By adopting these solutions, hospitals can enhance the efficiency and safety of their surgical operations.
Training and educating operating room staff on the importance of cord management is also essential. Ensuring that all team members understand the protocols and procedures for maintaining an organized surgical environment can help create a culture of safety and efficiency. Regular training sessions and assessments can reinforce best practices and keep cord management strategies top of mind.
Advancements in technology have also contributed to improved cord management in the operating room. New products like the Cord Management Drape are standardizing the cord management process and streamlining OR setup as a whole. Incorporating new technology into cord management strategies not only enhances organization and efficiency but can also keep patients safe from healthcare-associated infections. Hospitals can leverage new technologies to continuously refine their cord management protocols, ensuring they remain effective and up-to-date with the latest advancements.
Effective cord management is a critical component of maintaining a safe, efficient, and cost-effective operating room. By reducing surgical time, minimizing tool and cord replacements, speeding up setup and turnover, and decreasing infection risks, strategic cord management can have a significant positive impact on both patient outcomes and hospital finances.
As healthcare environments continue to evolve, hospitals must prioritize cord management as part of their broader efforts to enhance surgical safety and efficiency. By implementing standardized protocols, investing in specialized systems, and leveraging technology, hospitals can create an organized and effective surgical environment that benefits patients, caregivers, and the organization as a whole.
Ultimately, strategic cord management is not just about keeping cords tidy; it’s about improving the overall quality of care, reducing costs, and ensuring the best possible outcomes for patients. By taking a proactive approach to cord management, hospitals can position themselves for success in an increasingly complex and competitive healthcare landscape.

This is Part 1 in a 3-part series on strategic cord management in the operating room. In Part 1, we’ll offer an overview of the safety risks of...
This is Part 2 in a 3-part series on strategic cord management in the operating room. Part 1 offered an overview of the safety risks of poor cord...

The medical device industry moves fast—and it’s only getting more complex. Original Equipment Manufacturers (OEMs) are under constant pressure to...